
Mohammad Rahimi1, Mohammadreza Heidari2, Amirsaleh Abdollahi3*, Amin Ghanbarpour Juybari4 and Alireza Omrani Mazandaran5
1Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Mazandaran, Iran.
2Student Research Committee, Alborz University of Medical Sciences, Karaj, Iran.
3Medical Student Mazandaran University of Medical Sciences, Sari,Mazandaran, Iran.
4Anesthesiologist Mazandaran University of Medical Science, Sari, Iran Iran.
5University of Medical Science, Sari, Iran.
*Corresponding author: Amirsaleh Abdollahi, Medical Student Mazandaran University of Medical Sciences, Sari,Mazandaran, Iran.
Received Date: June 17, 2023
Accepted Date: July 01, 2023
Published Date: July 05, 2023
Citation: Mohammad Rahimi, Mohammadreza Heidari , Amirsaleh Abdollahi, Amin Ghanbarpour Juybari and Alireza Omrani Mazandaran. (2023) “Enhancing Acne Vulgaris Treatment: Innovative Non-Medication Approaches and Advanced Pain Management Strategies.” Case Reports International Journal, 1(1); DOI: 10.61148/CRIJ/005.
Copyright: © 2023 Amirsaleh Abdollahi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This review delves into innovative non-medication methods and advanced pain management strategies for optimizing acne vulgaris treatment while prioritizing patient comfort. Comedone extraction emerges as a valuable adjunctive therapy, particularly effective in treating open and closed macrocomedones. Cryotherapy, a foundational procedure since 1907, showcases significant success rates in healing inflammatory lesions and treating acne scars, surpassing traditional surgical methods.
Chemical peels offer a non-invasive solution, demonstrating substantial reduction in acne lesions, especially for mild to moderate cases. Microdermabrasion, subcision, dermabrasion, and optical treatments exhibit diverse mechanisms for effectively managing acne scars. Platelet-Rich Plasma (PRP) combined with microneedling and other modalities shows promising results in scar treatment, emphasizing its role in non-medication approaches.
Fractional radiofrequency and intralesional corticosteroids present safe and effective solutions for acne scars, with fractional radiofrequency showcasing potential as both monotherapy and combination treatment. Advanced pain management strategies, including selective nerve blocks, cryotherapy-anesthesia synergy, and intradermal anesthesia techniques, elevate procedural experiences while minimizing discomfort.
This comprehensive exploration underscores the efficacy of non-medication methods and advanced pain management strategies in acne vulgaris treatment, offering a holistic approach to enhance therapeutic outcomes and improve patient satisfaction.
Introduction:
acne vulgaris is a widespread and often persistent skin condition that affects a significant portion of the population, particularly during adolescence and young adulthood. The prevalence of acne is high, with up to 85% of individuals between the ages of 12 and 24 experiencing this condition. However, acne can also persist well into adulthood, affecting 64% of individuals in their 20s and 43% in their 30s. It is not only a cosmetic concern but can also have a substantial impact on individuals' self-esteem, social interactions, and overall quality of life. .[1]
The development and exacerbation of acne are influenced by various factors, including genetic predisposition, hormonal imbalances, nutrition, lifestyle, and skincare practices. Understanding these factors is essential for effective management and the development of targeted treatment approaches. [2-4]
Nutrition plays a significant role in acne development, with certain dietary components influencing sebum secretion and acne formation. Milk and its components, such as estrogen and insulin-like growth factor (IGF-1), have been found to affect sebum production, with IGF-1 stimulating sebum secretion and estrogen exerting a preventive effect on acne. Additionally, omega-3 and omega-6 fatty acids have shown therapeutic benefits in reducing sebum secretion and inhibiting inflammatory processes associated with acne. [5]
Lifestyle factors, such as stress and smoking, can also impact acne. Stress triggers the secretion of substance P, which influences sebaceous gland activity and sebum production. Smoking, on the other hand, affects skin microcirculation and alters sebum composition, potentially aggravating acne.[6]
Skincare practices and cosmetic use also play a role in acne management. While certain cosmetics may have comedogenic effects, appropriate skincare products containing anti-inflammatory ingredients can help minimize sebum production and contribute to the improvement of acne symptoms. [7]
Genetic factors and heredity have a strong influence on acne development. Studies on twins have demonstrated that identical twins have similar sebum secretion levels, highlighting the genetic component of acne. Additionally, factors such as alpha necrosis factor and gene activity in sebaceous glands have been associated with the occurrence of acne. [8]
When it comes to treatment options, a variety of topical agents and oral medications are available for managing acne lesions. Topical therapies, including retinoids (such as adapalene and tretinoin), antimicrobials like benzoyl peroxide and antibiotics, and other agents like azelaic acid and salicylic acid, have demonstrated efficacy in treating acne. Hormonal therapies, such as oral contraceptives, spironolactone, and clascoterone, have shown promise in managing hormonal acne. [9]
In addition to medication-based approaches, several non-medication methods can be employed for acne and acne scar treatment. These include comedone extraction, cryotherapy, chemical peels, microdermabrasion, subcision, dermabrasion, optical treatments (such as lasers and photodynamic therapy), platelet-rich plasma (PRP) therapy, microneedling, fractional radiofrequency, and intralesional corticosteroids. These methods offer a range of options that can be tailored to individual needs, with combinations often used to achieve the best possible outcomes. [10]
A comprehensive approach that considers the individual's characteristics, including the type and severity of acne, is crucial for successful acne management. It is important to consult with a healthcare professional, such as a dermatologist, to determine the most appropriate treatment plan based on individual circumstances and needs. Regular follow-up and adherence to treatment protocols are essential for achieving optimal results.
acne vulgaris is a common and often persistent skin condition that can have a significant impact on individuals' lives. By understanding the various factors contributing to acne development and employing a comprehensive and personalized approach to treatment, healthcare professionals can help alleviate the burden of acne and improve the quality of life for those affected by this condition
Non medication methods:
Comedone extraction:
One of the first physical methods of treating acne vulgaris is comedo extraction or comedone extraction. For patients taking topical and systemic medications, this technique is also helpful as an adjunctive therapy [11]. Lowney et al. were examined the effectiveness of comedone extraction in treating acne vulgaris on the forehead, cheeks, and chin in two experiments. These tests examined 20 and 12 people respectively. On the forehead, comedone extraction makes sense, but not so much on the cheeks [12]. Ramya et al., in a study that examined several treatment methods in comedonal acne, showed that comedone extraction was the most effective method in open comedones[13]. The treatment of Closed Macrocomedones can also be accomplished through comedone extraction [14, 15]. A small study of 30 patients using comedo extraction with trichloroacetic acid produced satisfactory results [16]. Various comedo extractors have been introduced for use in this method. In recent years, extractors have been introduced with different features, such as holes with different sizes and being disposable, so this method can perform better [17, 18].
Cryotherapy:
Cryotherapy or Cryosurgery is a basic procedure that uses a cold-temperature substance to affect the body. This method, which has been introduced in 1907, has been used in various fields, including acne vulgaris treatment [19-21]. Cryotherapy can be used to treat other types of acne, including acne Keloidalis and acne Conglobata[22,23]. This process has employed materials like solid carbon dioxide, liquid nitrogen, and liquid nitrous oxide. The advantage of cryotherapy seems to be the long-term healing of inflammatory lesions [11]. KARP et al. used cryotherapy on 50 patients to treat their acne scars and saw a 94% improvement in the patient's condition [19]. The success rates for papulopustular Acne and cystic Acne were 70 percent and 79 percent, respectively, in a cryotherapy study done by DOBES and KEIL in 95 individuals using the Slash method [24]. A study by WRIGHT and GROSS revealed that cryotherapy testing in over 2000 people was so successful that it replaced the surgical method they used [25]. Dobes examined the effects of cryotherapy on 120 patients with pustular acne and 58 patients with cystic acne and discovered that both groups displayed improvements of roughly 70% and 80%, respectively[10].
Chemical peels:
Chemical peels, also called chemexfoliation or chemical exfoliation, are procedures in which an abrasive chemical solution is applied to the skin for cosmetic or therapeutic purposes. They can be superficial, medium, or deep peels. This approach is used in various situations, including rosacea and acne vulgaris [26, 27]. To perform this typical non-invasive procedure, chemicals like mandelic acid, salicylic acid, lactic acid, glycolic acid, trichloroacetic acid, kojic acid, Jessner's solution and phenol are used [28]. There was no difference in the efficacy of the chemicals used in this procedure, according to a systematic review of 12 randomized clinical trials involving 387 participants [29]. Selecting the proper patient is an essential component of any chemical peel. The Fitzpatrick scale is frequently used to determine a patient's skin type. Other criteria, like a scale devised by Glogau, can also be used to identify patients. You should look up the patient's medical history before performing a chemical peel. For any chemical peeling, relative contraindications, such as pregnancy, should be taken into account [30]. According to a systematic review and meta-analysis conducted in 2022, the most effective treatment for mild to moderate acne was chemical peeling [31]. In another systematic review and meta-analysis conducted by de Vries et al., 11 studies investigated chemical peels and most of them reported a significant reduction in the number of acne lesions [32].
Microdermabrasion:
One of the most widely used ways to treat acne is microdermabrasion (MDA), a superficially invasive, non-chemical cosmetic procedure [33]. Microdermabrasion has been used for drug delivery in addition to cosmetic purposes. It is crucial to consider the patient's condition before using this method because it is contraindicated in some situations, such as infections [34]. In Lloyd's study, microdermabrasion was tested on 24 people, with over 70% showing good or excellent results [35]. In Arora's study, they investigated the effectiveness of microdermabrasion on acne scars. 100% of people with mild scars got excellent results, 88% with moderate scars got good or excellent results, and only 33% with severe scars got good results [36]. Microdermabrasion has been combined with other procedures. It has improved results when combined with adapalene and pyruvic acid, but not when combined with a 1,450 nm diode laser [37-39].
Subcision:
Subcision, also called incision-less surgery, is a simple procedure that can be easily combined with other acne scar treatments [40]. Dadkhahfar et al. reviewed 21 studies and noted the impact of subcision on acne scars and other scars [41]. Another review by Ahramiyanpour et al. compared needle-based and cannula-based subcision methods, and they showed that the two methods had similar effects on acne scars. They also mentioned studies using this method in combination with other methods of treating acne scars [42].
Dermabrasion:
Dermabrasion is a skin rejuvenation procedure that, when done correctly, produces dramatic results with few side effects. Dermabrasion still has some benefits over other modalities in some situations, even though its use has decreased as a result of the development of substitutes [43]. In a study by Roenigk et al. They considered the use of dermabrasion during and after administration of 13-cis-retinoic acid and observed no problems with wound healing or other problems [44]. Dermabrasion combined with regeneration technology using autologous skin cells has a remarkable effect on acne scars and expedites wound healing [45-47]. Aronson et al. conducted a study in which, dermabrasion was used on 25 patients, and the best results were seen on superficial scars [48].
Optical treatments:
There has long been interest in light and laser-based acne treatments that interfere with the pathogenesis of acne photochemically, thermally, or photoimmunologically. Light sources can be used alone or in combination with antibiotics or topical treatments [49]. Several visible and invisible wavelengths, or a combination of them, have been used to treat acne, but it is still unclear which has the best outcomes [50]. Acne vulgaris and its scars can be treated with a variety of sources, including infrared diode lasers, visible light sources (blue light, red light, blue-red light), pulsed dye lasers (PDL), intense pulsed light (IPL), potassium titanyl phosphate lasers (KTP), photodynamic therapy (PDT), nonablative lasers (e.g. Nd:YAG laser) and fractional ablative laser resurfacing (e.g. fractional CO2 laser, fractional Er:YAG laser) [51,52]. Numerous meta-analyses have been performed in the area of light sources and lasers, some of these analyses did not find any significant differences, such as when the red light and blue light source was compared to other treatments, the carbon dioxide fraction was compared to non-carbon dioxide laser treatments, Intense pulse light (IPL) versus other treatments and the pulsed dye laser (PDL) was compared to the control group [53-57]. On the other hand, some studies found that Photodynamic therapy (PDT) had more effects than other treatments [58].
Platelet-rich plasma (PRP):
Platelet-rich plasma (PRP) has been used in a variety of conditions since the 1980s, when the first reports of its clinical use appeared .[59] PRP is utilized for several aesthetic concerns, such as the treatment of acne scars and skin rejuvenation [60] Although this technique is widely combined with other methods such as microneedling [61], Subcision [62,63] , radiofrequency [64] and laser therapy [65] in the treatment of acne scars, it is also used alone in this case [66, 67]. The effects are better when PRP and microneedling are combined than when microneedling is done alone, according to Kang and Lu's meta-analysis [61]. Similarly to this, PRP and the Subcision technique worked better together [62, 63]. According to Al-aajem et al research, PRP and radiofrequency combination therapy for acne scars are both safe and effective [64]. Most research in the review study by Schoenberg et al. demonstrated that laser treatment and PRP combination produces significant clinical effects [65] 30 individuals with facial acne scars were included in the research by Gulanikar and Vidholkar, Regarding the decrease in scar size, PRP has showen a considerable improvement in all kinds of scars [66]. PRP was used on 20 patients in the research by Mikhael et al., and the results showed that it was effective [67]
Microneedling:
Microneedling is a treatment option that is used in the field of dermatology. It is a relatively new treatment option. The term "percutaneous collagen induction therapy" is another name for this treatment. It has been suggested that it could be used as a potential treatment for a wide range of conditions, such as melasma, acne scars, surgical scars, and skin rejuvenation, in addition to being used for transdermal drug delivery. It has been found to have a high degree of effectiveness while also being safe and having low post-treatment recovery rates. All of these factors have contributed to a rise in patient satisfaction and physician awareness [68]. This method is one of the safest methods that can be used to treat acne scars; the side effects that may occur as a result of using this method are relatively mild and are not harmful [69]. Microneedling was demonstrated to be a successful treatment for reducing the appearance of acne scars in a study that was conducted by Mujahid et al [70]. In the meta-analysis study by Shen et al., it was found that microneedling monotherapy is an appropriate and safe treatment option for acne scars that do not result in serious side effects [71].
Fractional Radiofrequency:
fractional radiofrequency is a treatment option for hyperhidrosis, as well as wrinkles and acne scars. Its mechanism works in a way that is similar to that of other forms of laser or phototherapy, fractional radiofrequency treatment induced intradermal heating working to inhibit the activity of sebaceous glands and promote the remodeling of the skin. The patient's clinical condition becomes better as a consequence [72]. Acne scars may be effectively treated with this procedure either through monotherapy or in combination with other treatments [73]. According to the findings of a recent study conducted by Li et al., individuals suffering from atrophic acne scars and active acne may find that the fractional radiofrequency method is a appropriate treatment [74]. It seems that treating acne scars with fractional radiofrequency is both safe and effective in treating acne scars. This technique makes it possible for neocollagenesis to take place with a reduced risk of post-inflammatory hyperpigmentation and other adverse effects that are generally seen in ablative and non-ablative lasers [75].
Intralesional corticosteroids:
Since the 1960s, patients with severe acne have been treated with corticosteroids administered intralesionally as a component of the usual treatment plan. In this procedure, triamcinolone acetonide is utilized most frequently [76]. According to the findings of a study that was published in 2020 by Gallagher et al. which examined the clinical practices of dermatologists, approximately 90% of whom have more than 10 years of experience, the majority of dermatologists treated acne with triamcinolone at a concentration of 2.5 mg/mL for more than 6 months. However, other concentrations and durations have also been used [77]. In the research conducted by Levin and Rasmussen, different concentrations of triamcinolone and betamethasone were treated in two separate studies on a total of 9 and 8 patients, respectively. The researchers found that the concentration of triamcinolone did not differ in terms of efficacy, whereas betamethasone did not have significant effects in comparison to the control group [78]. The usage of intralesional triamcinolone was explored in Leeming's study, and the results of recovery were seen to be satisfactory. The study included 27 patients who suffered from acne [76].
Non medication methods:
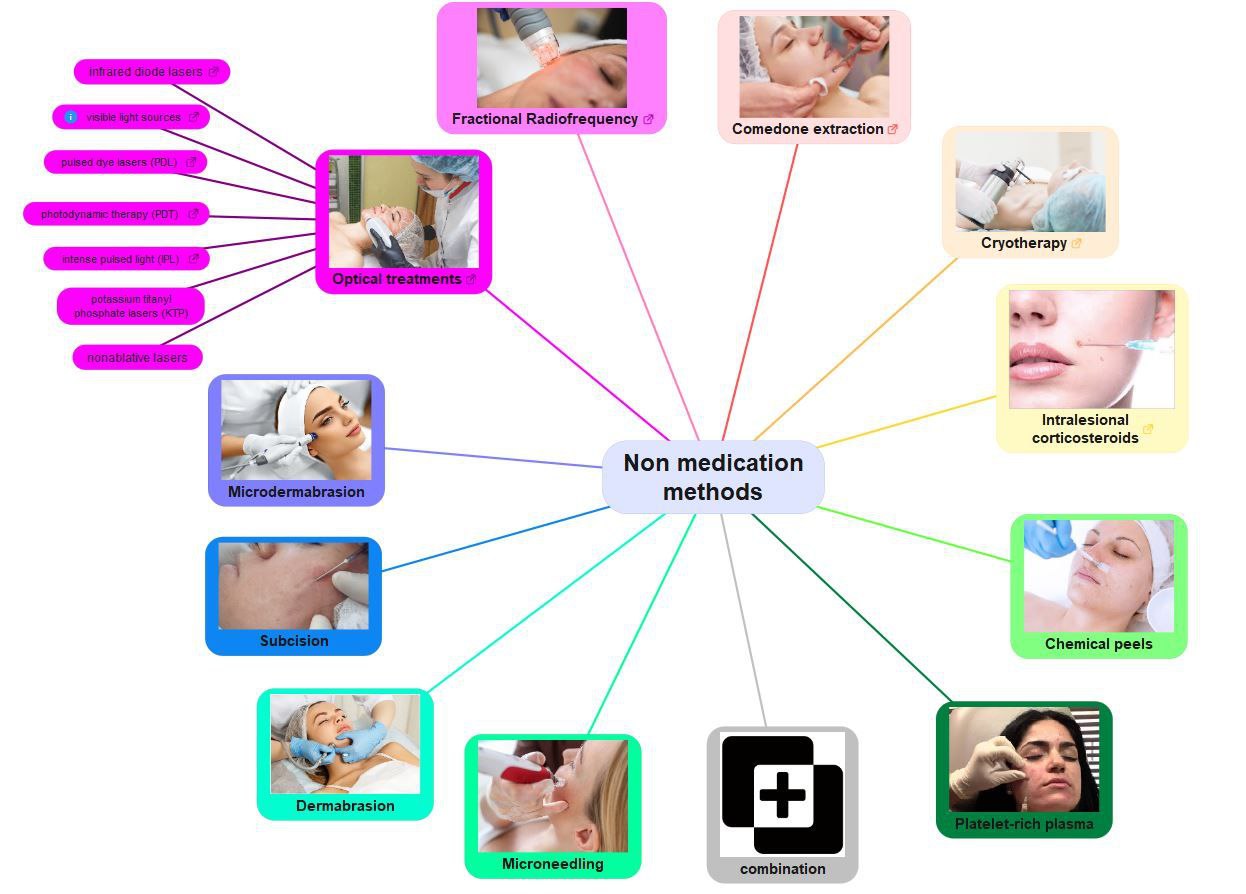
Figure 1: Non medication methods Acne, and specificially acne scars, can be treated using non-medication techniques that involve physical, optical, and occasionally chemical processes. Several of these treatments, including Comedone extraction, cryotherapy, and Intralesional corticosteroid injections have been used historically and are still employed today. In this context, other newer treatments such as microdermabrasion, microneedling, and platelet-rich plasma (PRP) are used. Additionally, these methods are often combined to increase their effectiveness. Figure 1 illustrates several Non medication methods.
Advanced Pain Management Strategies in Dermatological Procedures for Acne Vulgaris:
The meticulous integration of pain management strategies in dermatological interventions for acne vulgaris is an evolving domain, where precision and patient comfort intertwine. Beyond conventional local anesthetics, advanced techniques and considerations in pain management pave the way for enhanced procedural experiences.
Selective Nerve Blocks:
Incorporating selective nerve blocks tailored to the anatomical intricacies of the treatment site represents a refined approach. Targeting specific nerve pathways involved in transmitting pain signals allows for localized anesthesia, minimizing systemic effects. Dermatologists, in collaboration with anesthesiologists, can explore the feasibility of selective nerve blocks to optimize pain control in dermatological procedures. [79]
Cryotherapy-Anesthesia Synergy:
The fusion of cryotherapy with anesthesia presents an innovative avenue for pain management. Pre-cooling the treatment area with cryotherapy not only induces analgesia but also synergizes with subsequent local anesthetics, potentially reducing the overall anesthetic requirement. This dual modality approach showcases the evolving sophistication in pain management protocols for acne vulgaris interventions. [80]
Intradermal Anesthesia Techniques:
Advancements in intradermal anesthesia techniques offer a refined and site-specific approach. Intradermal injections of anesthetic agents directly into the dermal layer, either as bolus or via microinjection devices, enhance precision and reduce the potential for systemic absorption. This approach, when tailored to the requirements of dermatological procedures, contributes to an optimized pain management strategy. [81]
Ultrasound-Guided Anesthesia:
The integration of ultrasound guidance for anesthesia administration elevates precision in targeting specific tissue planes and nerve bundles. This technology allows real-time visualization, aiding in accurate deposition of local anesthetics. Dermatologists and anesthesiologists collaboratively harness ultrasound-guided techniques to augment pain management effectiveness while ensuring procedural accuracy [82].
Patient-Controlled Analgesia (PCA):
In scenarios where prolonged or post-procedural pain management is paramount, the implementation of patient-controlled analgesia offers patients a degree of autonomy. By allowing individuals to self-administer pre-determined doses of analgesics within safety parameters, PCA contributes to personalized pain management, aligning with the broader trend of patient-centered care. [83]
Psychological Analgesia Adjuncts:
Recognizing the psychosocial dimensions of pain perception, incorporating psychological analgesia adjuncts becomes integral. Mindfulness techniques, guided imagery, and cognitive-behavioral interventions contribute to pain modulation by addressing psychological components. Dermatologists, working in tandem with mental health professionals, can integrate these strategies into the pain management paradigm for acne interventions. [84]
Conclusion:
the following non-medication methods can be used to treat acne and acne scars:
Comedone extraction: This physical method involves manually removing comedones. It can be used as an adjunctive therapy alongside topical and systemic medications.
Cryotherapy: This procedure uses cold temperatures to treat acne and has been effective in improving inflammatory lesions.
Chemical peels: Various chemical solutions are applied to the skin to exfoliate and improve the appearance of acne. Different acids can be used, and chemical peels have shown significant reduction in acne lesions.
Microdermabrasion: This minimally invasive procedure involves exfoliating the skin using a device with tiny needles or a diamond-tipped wand. It has been effective in treating acne scars and improving skin texture.
Subcision: This technique is used to treat acne scars by breaking up fibrous bands beneath the skin, allowing the skin to lift and smoothen.
Dermabrasion: A more invasive procedure than microdermabrasion, dermabrasion involves removing the top layers of skin to improve acne scars. It has shown good results for superficial scars.
Optical treatments: Light and laser-based therapies, such as lasers of different wavelengths, intense pulsed light, and photodynamic therapy, have been used to treat acne and acne scars. Results vary depending on the specific treatment.
Platelet-rich plasma (PRP): PRP is used in combination with other methods like microneedling, subcision, radiofrequency, and laser therapy to improve acne scars. It has shown positive clinical effects.
Microneedling: This treatment involves creating controlled micro-injuries to the skin using tiny needles, stimulating collagen production and improving acne scars. It has shown good efficacy and safety.
Fractional radiofrequency: This treatment option utilizes radiofrequency energy to heat the skin and stimulate collagen production, improving acne scars. It can be used alone or in combination with other treatments.
Intralesional corticosteroids: Corticosteroids are injected directly into acne lesions to reduce inflammation and improve the appearance of acne. Triamcinolone acetonide is commonly used.
These non-medication methods offer various approaches to treating acne and acne scars. They can be used alone or in combination to achieve the best possible results based on individual needs and preferences